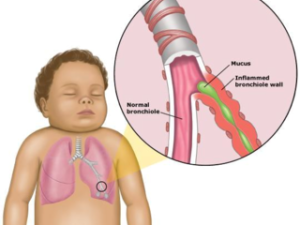
When Bug was discharged from the NICU after his 6 week early preemie birth, we were warned about RSV. Respiratory syncytial virus is a common infection that presents itself as a cold in older children and adults. However, in young babies around 2 or 3 months of age and especially in preemies in their first year of life, it can be very dangerous. RSV season is much like that of cold & flu so when Bug was almost 3 months old in June (1.5 months adjusted age), we didn’t worry about him contracting it.
Sunday, June 5, 2011: Bug had a bad cough and random bouts of wheezing. It got progressively worse throughout the evening, so we called our pediatrician’s after hours line. They recommended steaming the bathroom by running the shower and keeping the baby in there for a period of time, hoping it would break up any mucus that might be causing his symptoms. They also suggested using a humidifier in his room. There wasn’t any reason to give him Tylenol as he didn’t have a fever, and of course it’s no longer safe to give infants cold medicine. They said to watch for retraction of his ribcage, something we were very familiar with after our time in the NICU, and to check his breathing rate, both indicators of any difficulty he might be having breathing. They recommended a trip to the ER if he was struggling, especially since he was preemie who already had a compromised respiratory system.
We watched his ribs, measured his breathing, listened to his coughs and wheezes, and headed to the ER when we couldn’t stand it anymore. Of course, when they finally saw us in the ER, Bug didn’t feel like presenting any of his symptoms! The doctor listened to his chest and said he couldn’t hear anything in his lungs and thought it was just a bad cold. We requested a chest x-ray just to be sure, which came back negative for any signs of fluid or inflammation. They notified our pediatrician that we had been to the ER and what all went down, and set up a follow up appointment with them.
Monday, June 6, 2011: Daddy Bug took the day off from work as we only had a few hours of sleep the night before. He accompanied Bug and I to the pediatrician’s office, where he again didn’t present any of the symptoms that had worried us. At this point it seemed Bug only experienced them while he was sleeping, which would be typical for a cold. The pediatrician mentioned RSV and Bug’s increased susceptibility to it, but reassured us it was very unlikely and it was probably just a cold.
My parents had been away during the weekend and came home this afternoon. Before we could say anything, Mimi immediately heard the wheezing and asked us if Bug was alright. She kept asking if we were sure it was just a cold, and we assured her that both medical professionals we had seen thought so.
We set up his rocker/sleeper (he was still too small at this time to like sleeping in his crib) in our bedroom so we could listen to Bug while he slept again. He had stopped breastfeeding completely earlier in the day and wouldn’t take much from a bottle either, probably because it made his breathing worse. Late at night his breathing quickly took a turn for the worse, so after I told my parents were leaving, we took our second trip to the ER.
We ended up having the same ER doctor from our previous visit, who recognized us when he came to check out Bug. After a quick listen to his lungs, he said he didn’t need to do an x-ray to know it was bad. He asked us where we wanted to transfer Bug to since our hospital doesn’t have a pediatrics unit. We chose CHOP because we weren’t as familiar with the area around AI Dupont in Delaware. In the meantime, the nurses tried to set up an IV in case Bug needed meds intravenously. After several unsuccessful attempts with a too large IV (he was still newborn sized despite his age) and a screaming baby who cried himself out exhausted from the pain and being ill, we requested they stop. Bug had responded well to an albuterol breathing treatment they had given him earlier, and the ambulance was on its way for the transfer, so they decided to give up on the IV.

Bug received his albuterol by nebulizer. Like the baby shown here, he breathed in the mist that came out of the tube.
Tuesday, June 7, 2011: It was late enough that we saw midnight and beyond in the ER. We placed a call to my parents to give them an update, and they were so helpful. We asked if they could drop off a few important items (bottles, breast pump, milk baggies, pacifier, etc.) before we transferred to CHOP. They also brought snacks, water, and other things we didn’t think of during our quick leave. They came just in time to see Bug get packed up into a baby contraption that was then attached to a stretcher. The single image that stands out in my memory from this experience is Bug’s little round head, his baby face sucking away on his blue pacifier, his big eyes peering over the top of it, being wheeled out to the ambulance. To see such a little guy strapped to such a massive stretcher was humorous and awful all at the same time. He was so peaceful at that point and even smiled at one of the nurses.
I rode in the front of the ambulance (they don’t let you sit in the back?) and Jeff followed us in his car. I strained to keep looking through to the back of the ambulance; the only thing I could see was the back of Bug’s head. According to the nurses he looked around the ambulance for a little while and fell asleep, no crying or anything. We arrived at CHOP around 4:30am without any traffic or medical issues, and were quickly escorted up to our floor and checked into a room in no time. They even had our names written on the white board in our room, which was a comfort. They were ready for us.
The first order of business was checking out and making Bug comfortable, while I recounted his medical history and what all had occurred for us to be transferred to CHOP. I did my best but was so tired I had a hard time keeping the details straight. Everyone was wearing gowns, masks, and gloves so I was completely disoriented and couldn’t keep track of who was who. Plus I was super distracted because Bug was screaming bloody murder. They found he had a lot of mucus in his airways and were deep suctioning it out. This means they used a tube connected to a pump in the wall next to his hospital bed to suck out all the yuckies that were making it so hard for him to breath. And he wasn’t a fan, poor kiddo. They also swabbed his nose to run tests and discover what sort of infection he had developed. Meanwhile, Daddy Bug found parking and was looking for us. He said he knew he was in the right hallway and found our room because he recognized Bug’s screams. Another humorous and awful medical moment.
Our soon-to-be favorite nurse, Theresa, took me on a tour of the floor and showed me important things like where and how to store pumped breast milk, where they kept formula and Pedialyte, how they wanted me to keep track of Bug’s feedings, where we could do laundry, etc. Daddy Bug and I finally settled in around 5:30am after signing some paperwork. We were told that because Bug had responded so well to the albuterol treatments that they just wanted to keep him for observation and we would be able to go home most likely by the end of the day. We had a convertible couch in the room and were given a foldout bed, and were encouraged to sleep for as long as we could.
Daddy Bug was a real trooper and adventured into different floors of the hospital to find us meals and drinks. I stayed with Bug and reacquainted myself with all the awful monitors, equipment, and alarms we thought we had left behind for good at the NICU. As it turned out, Bug needed oxygen, regular albuterol treatments, and deep suctioning to keep his breathing regular and easy. We decided, after lots of struggling, that I would pump instead of breast feed so Bug could focus better on breathing. We met many doctors and nurses our first day, including a whole slew of specialists that visited each patient and their family for daily reports. We were included and encouraged to participate in these meetings to add any details we thought weren’t covered by our doctors or nurses. We found out at the end of the day that Bug tested positive for RSV, the one infection we hoped he wouldn’t have and were told was incredibly unlikely to develop. We were then told we weren’t checking out of the hospital this day.
Wednesday, June 8, 2011: Bug didn’t sleep well the night before, and neither did we. The doctors were trying to decrease the amount of oxygen he was being given, but he couldn’t breathe well enough to keep up his oxygen levels himself. This meant lots of alarms and not much sleep. He was diagnosed with bronchiolitis, which meant his breathing passages were so inflamed from RSV that he had difficulty breathing.
We met the respiratory therapist this day, who introduced us to chest percussion therapy. Basically you forcefully tap an instrument called a percussor across the baby’s chest or back to help them clear the mucus from their lungs. We enjoyed it because it was finally something we could do to help our baby.
It became clear that we weren’t checking out of the hospital this day either, but it was thought Bug would be better and check out the following day. Daddy Bug took a quick trip home to get his computer and other things he needed to keep track of work. Details spared, it was a crazy busy time of year and he had a lot of students, parents, and teacher he needed to coordinate and keep in touch with. Fortunately, he was able to stay at the hospital the entire time Bug had to be there.
Bug, never an easy sleeper to begin with, not only struggled sleeping this evening like he had before, but wouldn’t even go to sleep. Daddy Bug and I were going so crazy with our own fatigue at this point that the next time Nurse Theresa came to check in on Bug, we asked for her help. To this day, we don’t know exactly what she did, but involved flipping Bug to his back very quickly and giving him a gentle thump on his chest. He went to sleep almost instantly!
Thursday, June 9, 2011: Bug had finally gotten over the hump of his infection (RSV is notorious for the worst days of infection occurring between days 4 and 6). He was still wheezing but had lost the cough. He also required the extra oxygen and albuterol treatments like the days before. A respiratory technician came in to administer one of those treatments in the morning. It seemed like it was taking longer than the other treatments had but we think much of it. Sometime within the next hour, Bug’s lips turned blue (became cyanotic). We frantically called the nursing station. A nurse came running and saw his lips go cyanotic a second time just as the doctor entered the room. They treated him with a higher concentration of oxygen than what he was already breathing through his nasal cannula. They weren’t sure what caused it to happen, either his bronchiolitis or the albuterol treatment. Both Daddy Bug and I lost it at this point, wondering what else could happen.
Again, it was clear we weren’t going home this evening either. I called Aunt Lana, knowing she was coming into the city that evening anyway, and asked her to bring us changes of clothing, toiletries, nursing pads, etc. Again, we are so blessed by our family. She was so thoughtful and brought dinner, snacks, water, and even Bug’s favorite toy.
Bug improved throughout the day and we didn’t have any more cyanotic episodes. They gradually turned down his oxygen, even lower than where it was set earlier in the day. Alarms went off during the evening because he wasn’t breathing deeply enough to keep his blood properly oxygenated but that wasn’t any different than any of the other nights.
Friday, June 10, 2011: Daddy Bug and I were frustrated this day. Bug was better, not needing his nasal cannula during the day but still needing the extra oxygen at night, guaranteeing us another night at the hospital. We were going crazy with his monitor’s alarms, which kept going off for no reason at all. We learned how to temporarily mute it while we adjusted the pulse oximeter to go back on his toe properly. At one point, after a nurse checked on Bug, she very nicely told us to go to the food court and get out of the room awhile. The break was helpful but we didn’t stay away for too long. Our doctor came in the afternoon and said that if Bug did a good job with out oxygen that night, we would be discharged the following day!
Saturday, June 11, 2011: Bug did it – no oxygen the night before! We were discharged with an albuterol inhaler, breathing chamber, and mask. They showed us how to use it, when we should use it, and when it was necessary to go the ER should Bug have breathing issues again. They prescribed the inhaler because babies who have had RSV are at a greater risk for developing asthma or other respiratory problems when they’re sick in the future.

Waiting to be discharged.
We are lucky that RSV has been the only problem resulting from Bug’s prematurity. He hasn’t had any cognitive, physical, or developmental delays. He hasn’t had any further respiratory problems either, despite our insurance turning him down for Synagis, the monthly antibody shot that protects those at high risk for RSV during RSV season. They justified it because Bug doesn’t have any chronic lung or heart disease. All we could do was be thankful he doesn’t have any of those conditions. Anyhow, we are so blessed that Bug’s Story ends positively, when so many don’t.
To round out this third and final part of Bug’s Story, I’ve included our hospital bills below.
Thank goodness we were lucky enough to have good medical insurance and only had to pay a small portion of the following.
- ER (2 Visits) Total: $4,574.04
- CHOP (5 days) Total: $21,451.28
- NICU (15 Days) Total: $155,468.18